Understand
Digital Health Strategy: Serbia

Context
GDP: $USD 63,500 million
GDP per capita: $USD 9393.60
% of GDP spent on healthcare: 5.1
Population: 6.8 million
Life expectancy: 74.2 years
Gini co-efficient: 31.5
Geopolitical environment: Following war and upheavals, Western Balkan countries including Serbia began building economic and political systems in the early 2000s. Serbia is recognised as a European member state candidate country, a process that has since begun to accelerate again following recent war crimes by Russia on Ukraine. Work by the Centre for the 4th Industrial Revolution in Serbia has often led to best practice strategy development that addresses digitalisation across various sectors, open government approaches, and support for new economic activity.
Overview: Serbia's current digital health strategy
Name: Digitalisation program in the health system 2022-20261
Source: https://www.zdravlje.gov.rs/tekst/364590/program-digitalizacije-u-zdravstvenom-sistemu.php
Related documents:
- Annex and table of contents
- Action Plan for development of digitalization in health care for the period 2022-2023
- Draft law on health documentation and records in the field of health
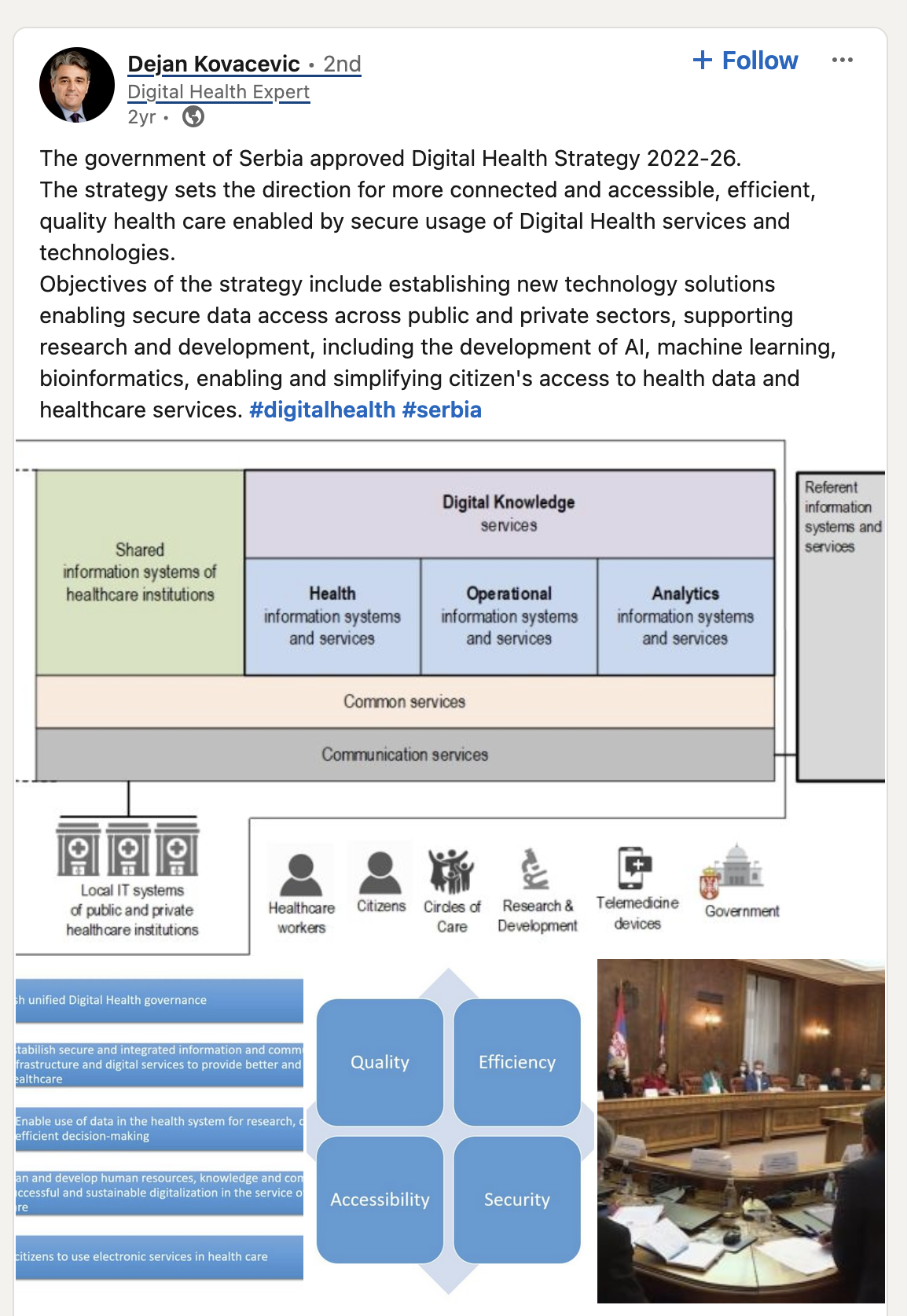
Components of the Serbian Digital Health Strategy
Organisational structure
Centralised: Health data systems are being created at the national level and aim to create a single digital health data repository that combines the National Institute of Public Health, Health Insurance Fund, Electronic Health Records (via Heliant), and the Medicines and Medical Devices Agency of Serbia. Plans are already identified for also incorporating the clinical genomic database. All up this will create a single health data agency similar to how Singapore has a national healthtech agency that manages healthcare data and builds analytics tools to improve planning, resource allocation and financing as well as assisting clinicians decide on treatment plans based on real world evidence.
Core national burden of disease datasets have been identified and over 70% of the population and 85% of healthcare providers make use of electronic healthcare records and a portal is available for citizens to access their healthcare data as well as share their own personal data from wellbeing apps and devices, if they wish.
In addition, healthcare service delivery was re-centralised in 2019 and is managed by the Ministry of Health for the entire country.
Use of regulatory levers
Current regulations have been proposed to define appropriate uses of health data for secondary purposes, that is for use in service planning, research, as real world evidence, and so on. Draft regulations were proposed some time ago, but this process was put on hold until the current Digital Health Strategy was prepared, and new work has now commenced to complete those regulations, as well as establish administrative and legislative arrangements for a health data access authority/body of some type that will oversee and authorise the use of health data across the Serbian digital health ecosystem. This work is expected to be completed this year.
Data governance processes
The core data systems aim to ensure interoperability and development of standards and a certification program for healthcare applications is part of the strategy, managed by an eHealth Steering Committee and technical working groups. A permanent working group has been established to define architecture and standards to increase the capacity for institutions like the National Public Health Institute in using and maintaining standards.
Best practice models for health technology assessment that incorporate real world data and evidence are also being designed. At present, this work is focused on speeding up approval chains for innovative drugs such as cancer treatments, for which there is a backlog, but it is expected that opportunities to assess and introduce new therapies, devices and healthtech apps for more preventative and upstream healthcare will be addressed in future years.
Data infrastructure
Implementation plans give clear targets for percentage of digitised systems expected, the hardware and software to be purchased, and mechanisms for exchanging data via APIs (For example, one implementation strategy notes “Establishment of legal and institutional processes for the purchase of machine readable data feeds from the health system in connection with analytics and notification, and anonymized and pseudo-anonymized data feeds, analytical services and notification.”)
Ecosystem approach
Serbia took a strong ecosystem approach to creating the Digital health Ecosystem, often hosting community consultations on Zoom, and including patient representative groups in a range of forums and working groups. Chambers of commerce, pharmaceutical and healthtech companies, public institutions, healthcare providers, research bodies and data protection authorities have all been involved in strategy planning and implementation working groups.
Outside of strategy implementation working groups, there also seemed limited focus on a program to foster ecosystem stakeholders to understand common data governance issues, define data sharing opportunities, and map relationships to better understand when to coordinate (such as on standards definitions and adoption), when to collaborate (to co-design and deliver new products and services) and when to compete (in a research and commercial marketplace).
Equity
While there were no clear discussions in the digital health strategy to discuss how data could be used to reduce health inequalities, aspects of the wider healthcare and service delivery strategy has prioritised some populations facing greater inequalities, such as specific preventative healthcare models and initiatives aimed at the Roma population. While Serbia proudly discusses following the Bismarck model, it is unclear how this translates to collecting data that would enable equity analysis. In the discussions on establishing the burden of disease and other clinical registers, it was unclear whether data to identify equity gaps are being sufficiently collected.
External studies, including by the World Bank and UNICEF were able to draw on a range of sources, including data from the Serbian Office of Statistics and Institute of Public Health to analyse health inequities and provide some recommendations for improvement.
Training/skills-building
Training and promotion focuses on informing patients of their rights to access electronic health records. We believe this should incorporate mechanisms where citizens can see on their healthcare records portal some data points/evidence that covers what value has been generated from their consent to sharing data (for example, population health improvements from clinicians able to use real world data, or from new research initiatives that have progressed thanks to sharing of data) as well space to discuss any potential vulnerabilities or data breaches and the actions/rectifications taken to reduce future risks.
Training and skills development for healthcare professionals to better implement data standards is reflected in targets focused on the monitoring of error rates and data validation levels in software solutions provided to capture and make use of electronic health records. It is presumed that this analytics data will help inform training and continuing areas of improvement in data quality management.
Funding and sustainability
Improving the financing of the healthcare system has been highlighted by World Bank and UNICEF in a 2022 study, and since this time, it appears this has become a priority focus. The digitization action plan includes several strategies and policy objectives that allocate funding to building data infrastructure, and a current reformation project focuses on improvement of financing in the healthcare system.
A healthcare panel hosted at the Kopaonik Business Forum in March 2024, with participation from the Health Insurance Fund, Roche, Center for the Fourth Industrial Revolution, Heliant and Platformable also focused on using data to make better healthcare financing decisions.
Serbia's Digital Health Strategy: In summary
A range of service improvements have been identified in various studies and efforts are underway to improve healthcare outcomes and service management across the country. Even just two years ago, reports were making recommendations on digitisation and modernisation and improvements for the use of health data to improve a range of outcomes including population health, reduced inequalities, service efficiency and planning, and to stimulate new economic industries.
Serbia’s Digitalisation Program in the Health System 2022-2026 is an excellent culmination of all of the work that needs to be done and draws on global best practices in planning the infrastructure and processes necessary to foster an open digital health ecosystem. Even more impressive is that since the strategy publication, a great deal of work has already been undertaken and progress continues at pace to foster a participatory and dynamic digital health ecosystem and to better collect and enable use of health data for the benefit of society.
Article references
Some of the initial reading done for this summary was also undertaken as part of the project Platformable did for the Open Data Institute, focused on mapping the maturity of secondary use of health data in the Western Balkans (https://secondary-use-health-data.theodi.org/tool/), and on a workshop conducted for ODI and Roche on the value of health data with ecosystem stakeholders (https://www.linkedin.com/posts/c4ir-rs_datasharing-healthtech-innovationinhealthcare-activity-7130555548525092864-dJNj/)
Mark Boyd
DIRECTORmark@platformable.com
Eric Rochman
EXTERNAL PARTNER