Understand
Digital Health Strategy: Australia

Context
GDP: $USD 1.693 Trillion
GDP per capita: $USD 65,099.80
% of GDP spent on healthcare: 10.65
Population: 26 million
Life expectancy: 83 years
Gini co-efficient: 0.34
UN Human Development Index Score: 0.946
Geopolitical environment: Australia is a wealthy, stable democratic country (although there is a monarchy still in place), with a Federal Government and state-based governments. Through the National Health Reform Agreements, the Federal Government collects taxes from citizens and then disburses funding to each state to deliver its own state-based health system. The National Health Reform Agreement stipulates how state funding is calculated for health service delivery, and defines national roles for health systems management. The next Federal election is due before November 2025. Despite its wealth, Australia has consistently failed to impact Aboriginal and Torres Strait Islander Health. In 2023, Australians voted against a referendum that would allow Aboriginal and Torres Strait Islanders to have a recognised voice in Federal Parliament.
Overview: Australia's current digital health strategy
Name: National Digital Health Strategy
Source: National Digital Health Strategy: 2023-2028
Related documents:
- National Digital Health Strategy 2023-2028: Delivery Roadmap
- Intergovernmental Agreement on National Digital Health 2023-2027 (IGA)
- Connecting Australian Healthcare – National Healthcare Interoperability Plan 2023–2028
- Clinical Governance Framework for Digital Health
Components of the Australia Digital Health Strategy
Organizational structure
Centralised and federated hybrid model: Australia's first digital health strategy was released in 2017 with the most recent iteration building upon the accomplishments achieved since its initial release. The most recent version lays out a comprehensive plan that includes a 5-year delivery roadmap which is under the direction of the Australian Digital Health. The vision of the National Digital Health Strategy is “an inclusive, sustainable and healthier future for all Australians through a connected and digitally enabled health system”. The core focus of this next phase of the digital health strategy is to improve how information is shared across the health system, to implement real-time data exchange so that individual and aggregate-level health information is readily available while taking into consideration the importance of consumer consent and using strong privacy and cybersecurity standards.
Throughout the strategy, Australia weaves in innovation to drive improvements in care to develop a person-centered digital health system that works for all partners and collaborators through an equity-focused approach.
To achieve the digital health transformation nationally, the strategy identifies four change enablers that reflect existing areas within the digital health ecosystem that require consistent and ongoing effort to achieve the desired outcomes. The four change enablers are:
- Policy and regulatory settings that cultivate digital health adoption, use and innovation
- Secure, fit-for-purpose and connected digital solutions
- Digitally ready and enabled health and well-being workforce
- Informed, confident consumers and carers with strong digital health literacy.
These change enablers are identified as necessary components to achieve the following outcomes:
- Digitally Enabled: Health and wellbeing services are connected, safe, secure and sustainable
- Person Centered: Health and wellbeing services are connected, safe, secure and sustainable
- Inclusive: Australians have equitable access to health services, when and where they need them
- Data-driven: Readily available data informs decision making at the individual, community and national level, contributing to a sustainable health system.
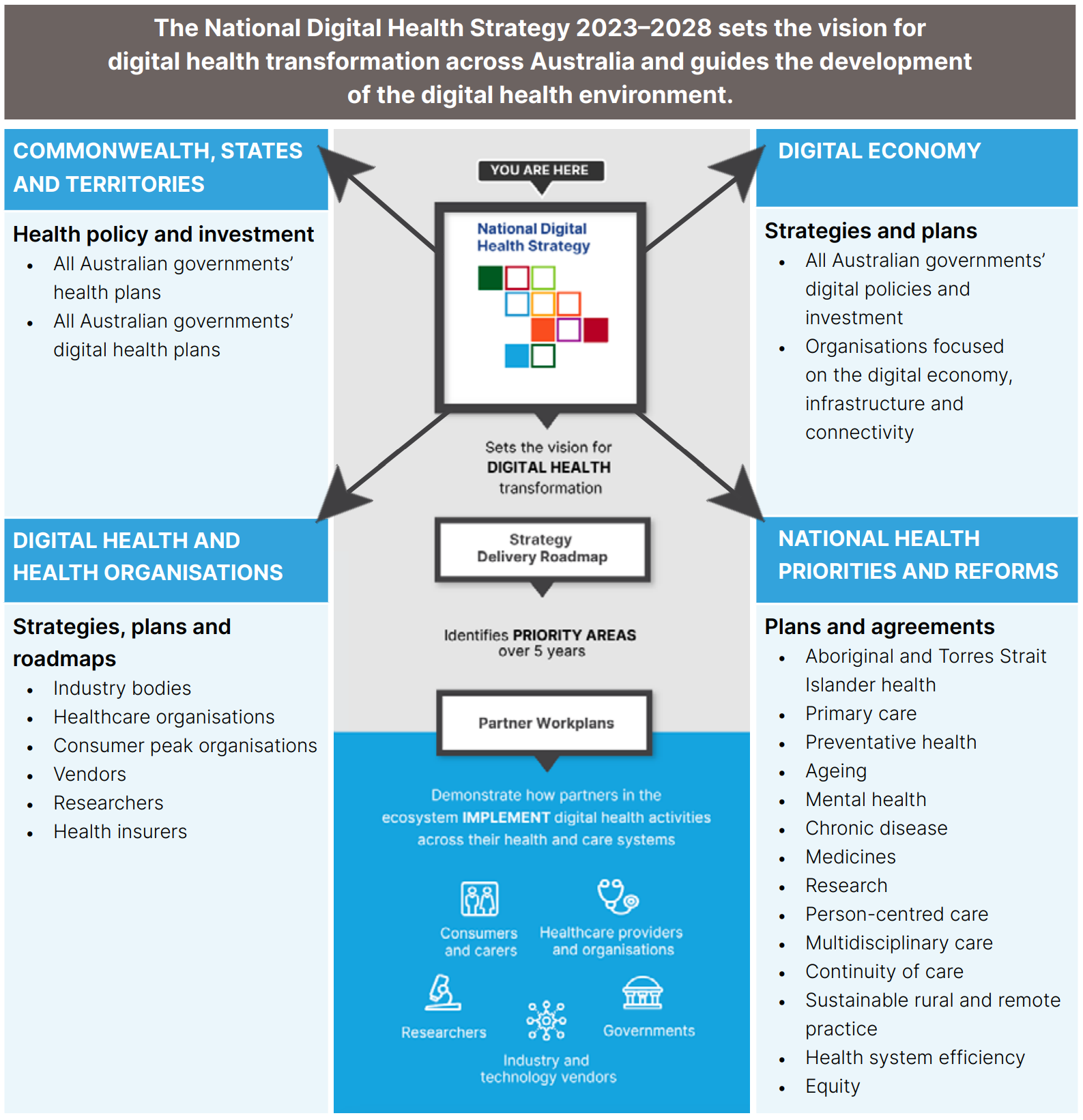
A common theme throughout the strategy is the acknowledgment that partnership and collaboration across the various players in the digital health ecosystem is critical to long-term success.
The categories of partners identified in the strategy match Platformable’s ecosystem model of stakeholders and includes:
- Consumers and carers
- Healthcare providers and organisations
- Industry and technology vendors
- Researchers, and
- Governments.
The Strategy Delivery Roadmap identifies 12 priority areas, as shown in the image below.
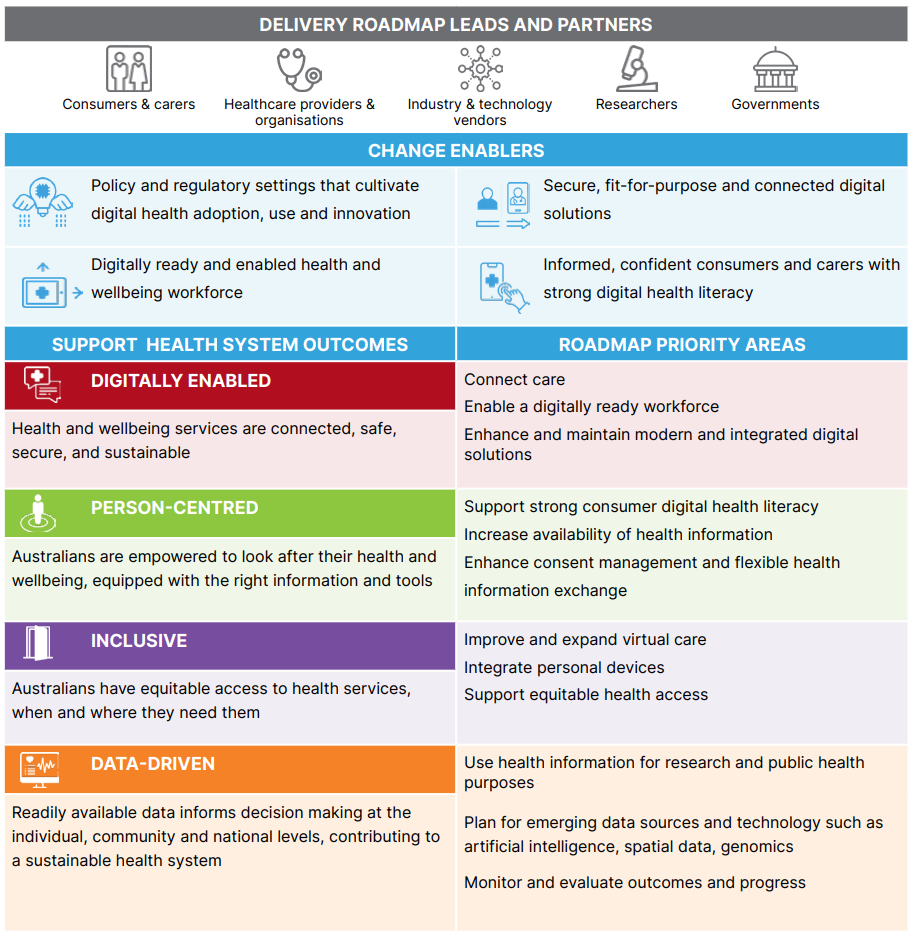
The current status of each roadmap priority area is defined in order to encourage ecosystem stakeholders to plug into work programs and is aimed at supporting better coordination and collaboration amongst players.
This approach enables a centralised and federated approach to healthcare: digital health systems are centralised nationally through interoperable data standards and data models, data infrastructure, data governance and literacy training and tooling, while data collection at point of healthcare delivery is managed by state health systems.
Governance
The core organising body for the strategy is the Australian Digital Health Agency, under the direction of the Commonwealth, state and territory Health Ministers. The Agency Board must approve the strategy before it is disseminated to the Health Ministers, and is responsible for the ongoing governance of its implementation.
Organisations identified as ‘leads’ within the roadmap hold the responsibility of implementing and coordinating the activities with partner organisations utilising an existing advisory and governance structure. To ensure transparency, progress is provided to the Agency’s Jurisdictional Advisory Committee and its Board. Any proposed amendments for the roadmap are required to gain approval from the Agency Board in accordance with Commonwealth, state, and territorial health ministers and other relevant agreements such as the Intergovernmental Agreement on National Digital Health 2023-2027 (IGA).

Use of regulatory levers
Regulations supporting the implementation of a cohesive national digital health ecosystem include:
- The Australian My Health Record is a national electronic health record system that enables citizen access to their health records while ensuring clinical information can be shared securely with consent
- The Privacy Act 1988 addresses cybersecurity and resilience measures and supports the protection of personal health information.
The strategy urges stakeholders to embrace innovations and cutting-edge technologies including AI, machine learning, big data analytics, and quantum technology. The need for collaborative development of policies and regulatory frameworks to manage potential risks that these technologies bring to the healthcare landscape is recognised.
Data governance processes
Incorporated into the digital health strategy is the Connecting Australian Healthcare – National Healthcare Interoperability Plan 2023–2028 which establishes the vision for the safe and seamless sharing of consumer health information through five priority areas related to identity, standards, information sharing, innovation, and measuring benefits. The implementation of the plan is supported by The Council for Connected Care (CCC) which is tasked with identifying opportunities to improve and adopt interoperability across the healthcare system.
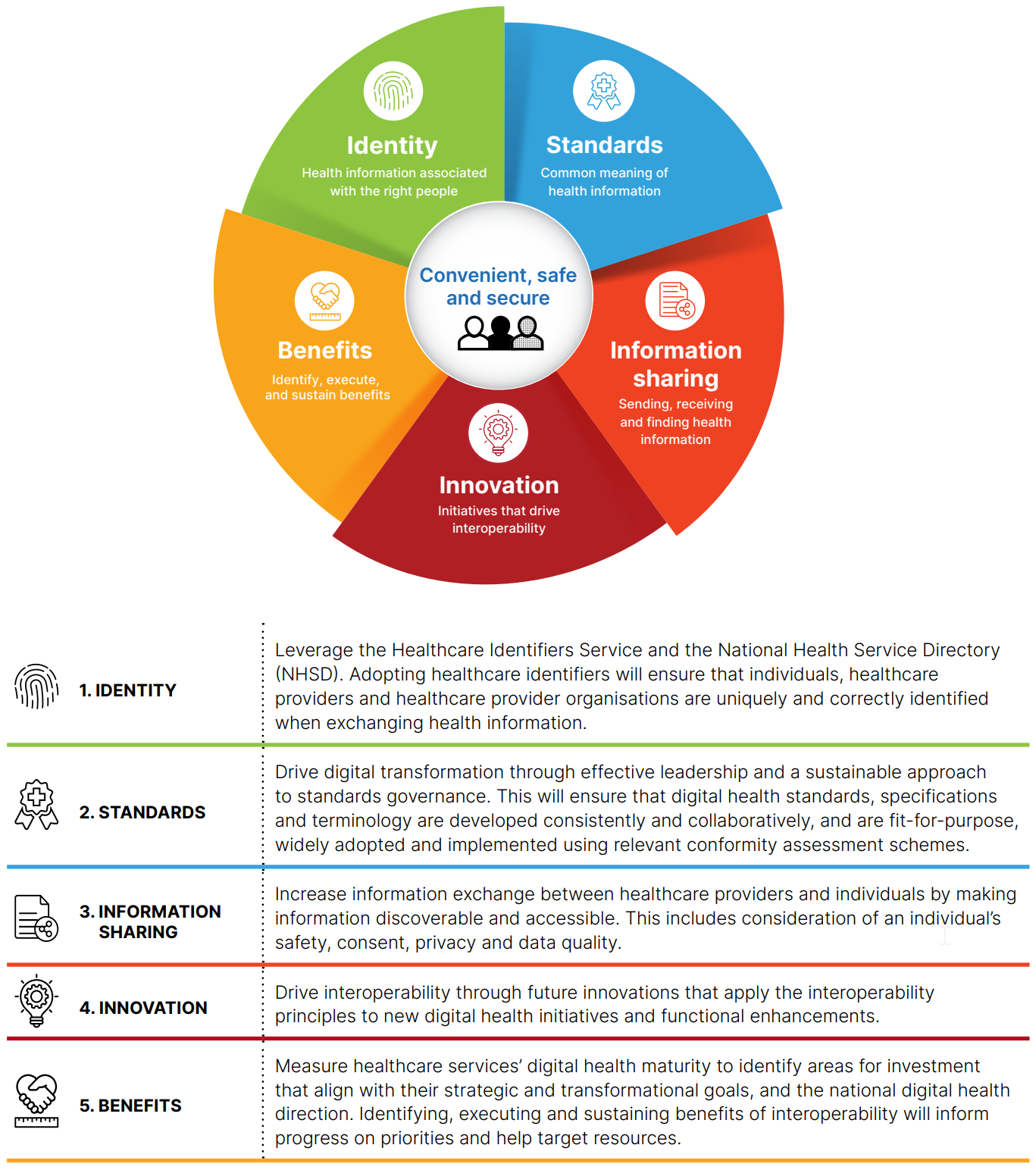
Digital health standards are a necessity in this digital health ecosystem. Standards are seen as a technical foundation: necessary for the safe, secure, timely, and accurate sharing of information. In particular, the use of international standards is identified as a way to provide assurance to partners in the healthcare industry that their products and services can compete globally and remain relevant in markets outside of Australia.
Two standards that are mentioned in the digital health strategy are:
- National Safety and Quality Health Service (NSQHS) Standards: developed collaboratively to support the implementation of a clinical governance framework with the goal of improving the quality and reliability of health services while protecting consumers.
- Fast Healthcare Interoperability Resources (FHIR®): an open standard that provides free access to technical specifications, industry partners, and implementation support.
Data infrastructure
The modernisation of digital infrastructure supports quality care and enables providers to access and share the right information when they need it. Implementation of digital solutions that seamlessly integrate into clinical workflows, are easy to use, and ensure clinical quality and safety are necessary to enable the sharing of information and high-quality data that support improvements to health outcomes. The pathway and actions to create a digital ecosystem of connected providers are included in the Interoperability Plan.
Improvements to digital infrastructure also lead to increased productivity of the healthcare workforce. The strategy defines the creation of a single view of an individual that compiles data from sources across the healthcare system to allow health information to be securely shared, discovered, and combined. Breaking down silos of information and clinical documentation to real-time data exchange in a consolidated format will allow healthcare providers to respond to the needs of consumers as they transition across different healthcare settings such as primary care, acute care, and aged care.
The strategy recognises that to achieve its goals, and to enable more technological solutions, also requires a robust digital infrastructure to be in place across the continent with access to reliable and high-speed internet and mobile connectivity in remote and rural regions of the country.
Ecosystem approach
Australia's strong ecosystem approach to its digital health strategy engages a wide range of stakeholders to contribute to the development and ongoing implementation. Collaboration by all partners including consumers and carers, healthcare providers, industry and technology vendors, researchers and academia, and governmental institutions is considered a key factor for long-term success. The strategy suggests the creation of a culture of cooperation and engagement across all partners both through formal structures, organisations and bodies, and also through informal relationships that help drive collaboration and innovation. But overall the roadmap and documents do not describe how this will be fostered in new ways or using new structural approaches at present.
Gaining the confidence and trust of all the stakeholders involved in the healthcare system is critical for successful adoption. Enabling consumers to have trust and confidence in using digital technologies that enable access to reliable and transparent information is incorporated through the framework and considered in how initiatives are developed and implemented.
A unique aspect of Australias Digital Health Strategy is the emphasis on marrying digital health product development with clinical governance, which is further defined in the Clinical Governance Framework for Digital Health. The framework establishes five principles that are considered critical factors in developing digital health products and services. The five principles included in the framework are:
- Leading with our people
- System safety and quality improvement
- Evidence-based practice
- Person-centredness
- Partnership
This combination of clinical governance with digital health governance ensures that the technology meets the objectives of clinical care and outcomes and strengthens the consideration of how technology can be used to enhance clinical workflows. At Platformable, we take a similar approach to how we apply a program logic model thinking to the development of health data governance frameworks, ensuring that the data that is collected and utilized supports the outcomes and impacts of the initiatives being implemented.
Equity
The importance of taking an equity-based approach is directly addressed throughout the strategy, acknowledging the importance of supporting and improving the health and accessibility of marginalised and minority populations. All digitally enabled health and wellbeing services must be culturally sensitive and appropriate for all individuals, including Aboriginal and Torres Strait Islander peoples, peoples from culturally and linguistically diverse (CALD) and LGBTIQ+ communities, as well as members of all religions. The person-centred outcome specifically mentions:
- Support the implementation of the National Agreement on Closing the Gap, providing greater access to culturally safe and responsive health services for Aboriginal and Torres Strait Islander peoples
- Improve health outcomes for parents and children in the first 2,000 days of life
- Reduce access barriers experienced by LGBTIQ+ people
- Support trauma-informed care for veterans and their families
- Support older people to age well in either their own homes or residential aged care facilities
- Develop solutions that help prevent and manage chronic health conditions
- Support the provision of culturally safe health services for Australia’s diverse populations
- Help overcome the challenges of healthcare in remote and regional areas
- Support appropriate and accessible healthcare for people with disability.
The measurements for success include equity as one of its metrics through the strategy's ability to address inequities in the healthcare system and ensure that the diversity of individuals' needs is met.
Training/skills-building
Equipping the healthcare workforce with the skills to promote and utilise digitally enabled tools is one of the four change enablers. Only through an engaged and confident workforce that embraces digital health solutions will the benefits be achieved for the consumers. Investing the time and resources to train the workforce to improve the adoption of digital tools and infrastructure achieves the efficiency of implementing digital health solutions. Capacity and skills-building on digital health solutions are integrated throughout health and care education, accreditation, and training, including across all fields of healthcare such as medical, nursing, disability, aged care, mental health, and allied health fields.
Improving the digital health literacy of consumers and carers to ensure they are informed and confident in their abilities to utilise digital health tools is identified as a change enabler. Both health literacy- defined as “being able to understand and apply the health information provided to individuals'' and digital literacy- “being able to understand and apply digital tools” are integral to the uptake and engagement of consumers and carers so that they can participate fully and equitably. Incorporated into the person-centred outcome of the roadmap is the support for strong consumer digital health literacy as a priority area and calls on all stakeholders to take an active role in the design and delivery of digital literacy programs and initiatives that are evidence-based and incorporate best practices.
Funding and sustainability
The strategy identifies the need to incorporate agile funding agreements across the Commonwealth, states, and territories to achieve the digital health reforms required to support the rapidly changing environment. The Intergovernmental Agreement on National Digital Health 2023-2027 (IGA) supports funding for the National Digital Health Strategy however additional funding from public, private, and not-for-profit sectors is needed. The National Digital Health Survey conducted in 2021 identified that 52% of healthcare providers indicated that cost was a key barrier to the adoption and use of digital health tools in their day-to-day work activities. In addition, affordability is a concern amongst consumers, preventing 10% of consumers from using digital health.
While these concerns are identified, the strategy does not provide any direct plans for how it intends to address these issues. It does acknowledge however that while the implementation of digital health may require an upfront investment, it can deliver more effective and efficient care at a lower cost, including through the reduction in administrative burden, overservicing, and duplication.
There is substantial evidence showing that investing in digital health leads to better system sustainability, with the need to identify how to better understand and measure this benefit. Sustainability has been incorporated into the measurements of success for the digital health strategy however it is not clear how the strategy aims to address and ensure the long-term sustainability of its activities and initiatives.
Summary
Australia’s digital health strategy provides a well-defined plan through a comprehensive and holistic approach to developing and implementing digital health initiatives and activities that will achieve key outcomes in improving the delivery and access to care with the ultimate goal of creating a truly person-centred healthcare system. Its ecosystem approach to engaging stakeholders across the healthcare sector to act as partners and the identification of the key priority areas and the initiatives for which partners can contribute to its success establishes a clear path to improve the digital health infrastructure and increase the engagement of consumers. The strong equity focus is imperative to create a healthcare system that accounts for and serves the varying diversity and needs of the population, creating a more accessible system that provisions care equally to all who need it. Australia is a strong example of a digital health strategy that is preparing its healthcare system for the future by taking a forward-thinking approach in its development of key infrastructure and training of its workforce to digitally enable its health system.

Eric Rochman
EXTERNAL PARTNER