Engage
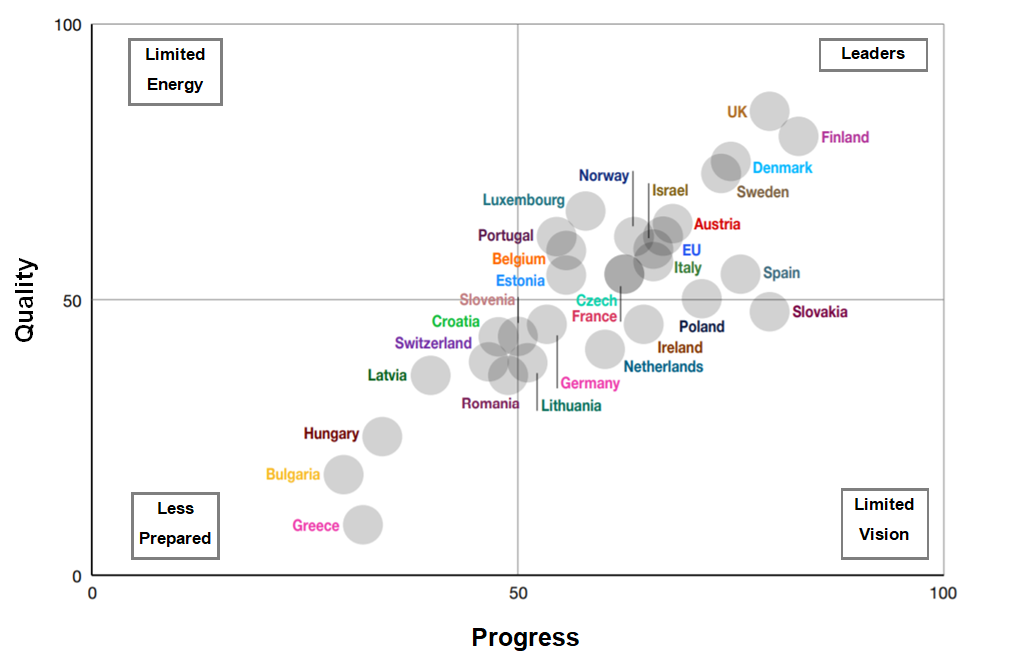
How advanced is the open health data ecosystem in Europe?

The need to optimise health care systems and reduce unequal health burden is critical. The global pandemic has also spurred policy makers, health professionals, and researchers to improve health data collection, sharing and use.
The Open Data Institute engaged Mark Boyd as a freelance researcher/writer (Senior Policy Associate) working with the wider ODI team (that included Dr Mahlet Zimeta, Dr Jeni Tennison and Mahad Alassow all from the ODI) on independent research sponsored by Roche, to measure the potential for using health data for secondary purposes across Europe.
For this study, we researched the literature and categorised key benefits from secondary use of health data into four groupings, as shown below. This was then validated with project participants.
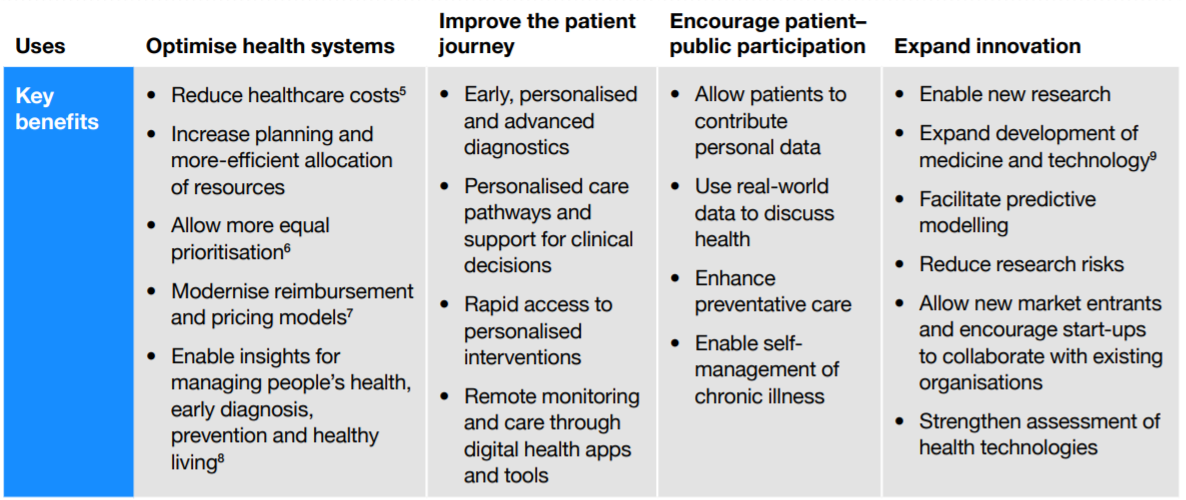
Creating a policy framework to analyse health data ecosystem maturity
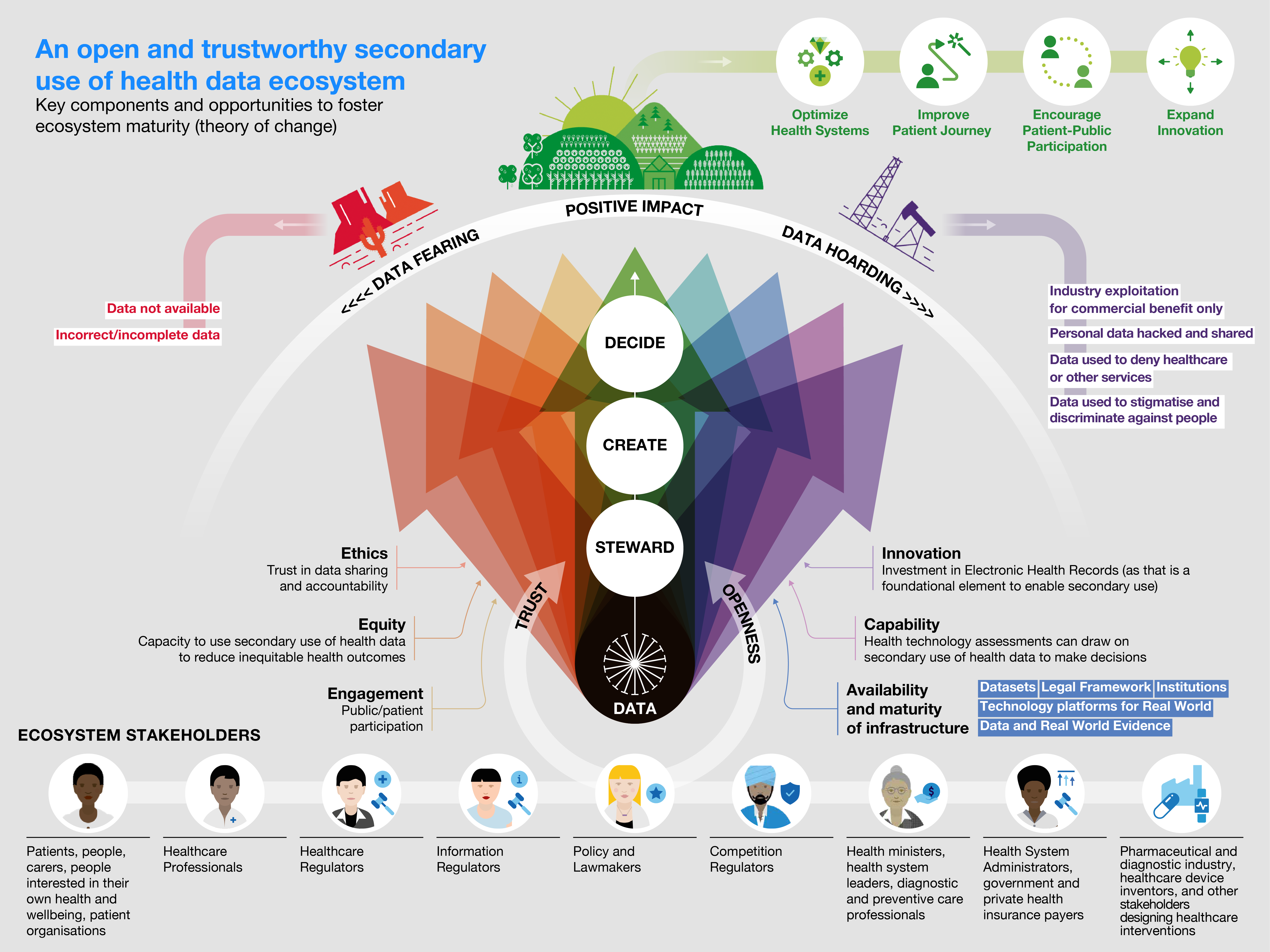
The Open Data Institute's project defined a policy framework that could be used to assess the maturity of health data ecosystems in Europe (at the regional or country level).
By assessing the policy maturity, it is possible to identify the areas where each country (and Europe as a whole) can improve the health data infrastructure, relationships, and other data governance supports to ensure a greater likelihood of open ecosystems generating value from health data while protecting data privacy rights.
To create the policy framework, we drew on the ODI’s theory of change and applied it to health data ecosystems, in particular. The ODI theory of change recognises that for data to have a positive impact, it requires a multi-stakeholder network collaborating to ensure key components are in place: infrastructure, capabilities, innovation, ethics, equity and engagement. Using this theory of change, we could define the key characteristics under each of these components that needs to be in place to generate value from health data.
Secondary use of health data policy framework
The ODI identified 22 key policy components, based on the ODI's manifesto for elements of open and trustworthy data ecosystems. For each, a success indicator defined how the component would operate as a fully functional policy area. These indicators were then evaluated in order to create a European-wide scorecard and profile. These profiles included policy challenges, policy achievements, and best practice highlights for each country. Individual scorecards and profiles were created for 25 EU member states, and 4 non-EU countries (Israel, Norway, Switzerland, and the UK).
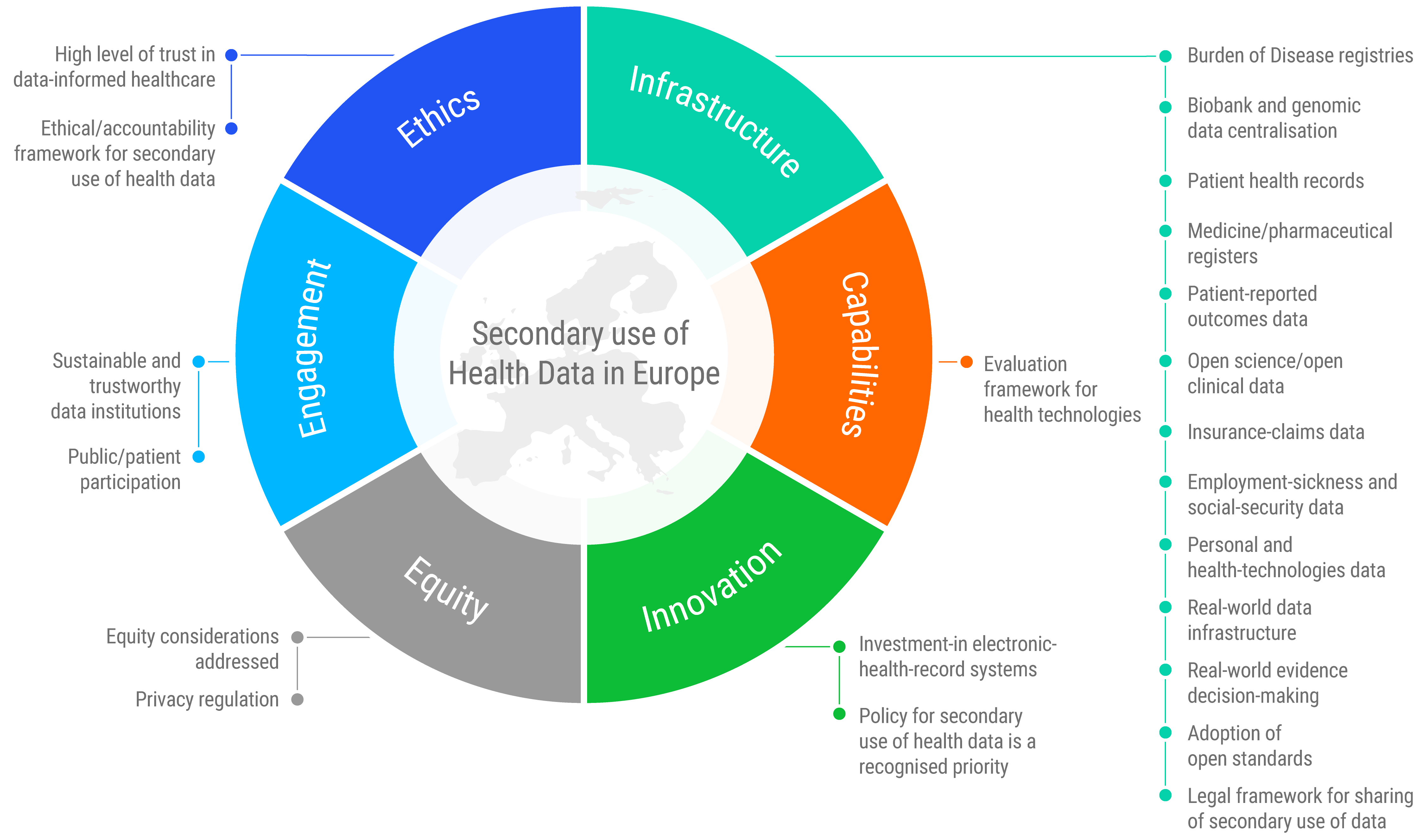
The interactive comparison tool created from the country scorecards allows users to easily rank and compare countries across different policy areas. This allows policy-makers to compare themselves with peers and identify good practice approaches to follow and adapt to their local contexts.
Enabling secondary use of health data is the cornerstone of creating an open health ecosystem
The ODI's project and report found that overall, Europe is making progress on enabling secondary use of health data. If used securely and ethically, this data could improve health outcomes by supporting stakeholders to solve complex challenges collaboratively, foster new economic opportunities, and ensure everyone can participate and co-create in the open health ecosystem.
But while health data policy environments are encouraging greater secondary use and data sharing, the ODI's project found that many initiatives are still fragmented. Significant work is still needed to establish strong health data ecosystems and infrastructure.
Four of the biggest challenges that remain, as identified by the ODI's research, are:
- Lack of clarity on how to apply the European General Data Protection Regulation (GDPR) to enable secondary use of health data while maintaining strong data privacy and protections
- Fragmented initiatives and approaches hindering each country’s ability to support each other or encourage widespread participation
- Lack of agreement on common data models and open standards. This creates barriers for interoperability and reuse of health data
- Limited focus and priority on identifying opportunities to use secondary health data to reduce health inequalities.
Building trust
Platformable's reflection on this project and research considered the challenges of building trust in sharing and use of health data. The following discussion is our own thoughts on the research and was not part of the ODI's project:
Fostering a trustworthy health data ecosystem requires a great deal of trust by patients and people generally, by healthcare professionals, and by stakeholders looking to create partnerships or to compete in the market.
The components identified in the policy framework - the data infrastructures and other policy supports - won’t make a difference to health outcomes and the use of data unless stakeholders bring the community along at each step of the way. Data governance mechanisms are essential for creating a trustworthy health data ecosystem, because governance ensures oversight, accountability, and implementation of best practices that strengthen the processes around health data sharing to protect everyone.
But data governance processes are not enough. As the research shows, countries with a solid data infrastructure - like the UK - can still take serious missteps - as they did with announcing the sharing of the whole population’s health data earlier this year - which can destroy community trust in health data ecosystems going forward. There is a need for each country and Europe as a whole to create a dialogue with the community generally and with patient representative groups to discuss how to ensure societal benefits from the reuse of data, while also protecting individual data privacy.
Proposing a new model of Continuous Engagement / Continuous Consent
At Platformable, we see that in tech circles, when we talk about keeping applications and websites up-to-date and always available, we talk about a process called continuous integration/continuous development. It refers to a “DevOps” cycle whereby as code gets built for a new digital product or for a new feature within an existing app, it goes through a process of being tested against the existing codebase to make sure it doesn’t break anything and that it is secure and doesn’t create new vulnerabilities. This new code then gets pushed to deployment in a constant loop of improvement.
Our reflections on the ODI research and project lead us at Platformable to consider the need for a similar model in how health data is discussed and used: a process of continuous engagement, whereby every step of the way, health data ecosystem leaders and other stakeholders communicate the use of health data, share the value that is being generated, and describe how the risks and vulnerabilities are being addressed.
This continuous engagement could help address one of the current unresolved challenges in working with community members around opening health data: consent flows. Under current systems in Europe, individual consent is needed each time that someone agrees to provide the use of their health data for a particular purpose beyond primary care (and even then, consent is sometimes needed to share data between healthcare professionals).
Solutions to enabling a health data ecosystem can’t rely on people sitting there toggling a hundred or more individual approvals for use of their health data in some sort of app settings screen.
But equally, people are (rightly) reluctant to agree to sharing their health data for ‘exploratory’ reasons with commercial providers who say they want to use the data for health research. When it is open-ended, what would stop a commercial provider sharing that data with health insurance or other companies that have proven to play a role in limiting access to health services based on current health status?
There needs to be a new level of consent that sits somewhere between the granular approval for each and every case of data use on one side, and the carte blanche opening of health data in a manner that reduces the accountability and oversight of health data users, on the other.
One model could be to create research agenda templates that people can agree to: where specific research use cases are stipulated, people could consent to share their data with trusted stakeholders to make use of their personal (anonymised) health data to advance those research goals, and not for open-ended exploration. Other consent characteristics, like enabling data sharing where it would help advance rare disease therapies, or to share data only with specific actors, such as non-profit research institutions, and so on, could be created to enable patients to share their data more widely, but within set parameters that reflect their concerns, ethics, and values.
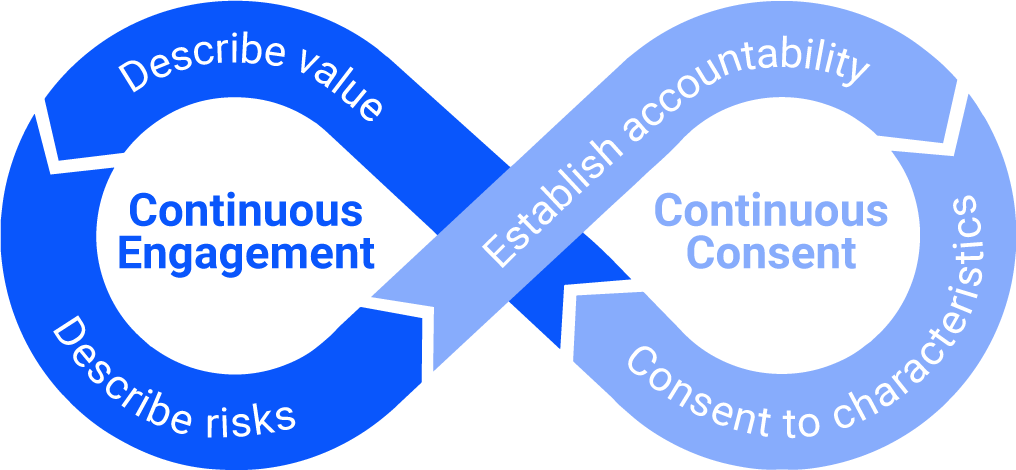
A proposed approach to continuous engagement/continuous consent for building a trustworthy health data ecosystem (Source: Platformable's elaboration)
At Platformable, we plan to further explore what a new model of continuous engagement/continuous consent would look like that enables use of health data responsibly and ethically. We will also be continuing our work developing data governance tools, policy briefs, and products for community health organisations, in particular. For example, our partnership with Black Health in the United States focuses on building data governance systems and policy solutions that aim to address health inequities facing African American and Latinx communities in New York City and across the United States.
To find out more about our data governance products and training services, contact us or visit our Data Governance pages.
Mark Boyd
DIRECTORmark@platformable.com